"Change is inevitable. Growth is optional.” John Maxwell
Over the last decade, healthcare has undergone significant changes, not the least being a consequence of digital transformation.
Digital health solutions have the potential to improve healthcare delivery in radical ways and serve to deliver value based care, by driving better efficiencies and better patient outcomes. Despite this, implementing meaningful change through digital transformation can be both challenging and frustrating.
New digital projects invariably impact the daily routine of the healthcare workforce, and in reality, most of us would rather avoid change if possible. Embracing change, however, is an important part of growing your organisation, remaining relevant and building a competitive edge.
Successful software implementation within your healthcare organisation is as dependent on the quality of your change management process as it is on the technology itself.
In this article, we uncover the fundamental elements of successful software implementation within your organisation. Whether you are Head of IT in a large organisation, a clinical leader or practice owner or manager in a small practice, adopting these principles will help your organisation or practice get the most out of its technology investment, keep your staff engaged and happy and deliver better outcomes for your patients and your organisation.
1. Understand and leverage user adoption profiles within your organisation
Have you ever wanted to implement a great new digital solution to your healthcare team knowing that it is going to improve patient safety, improve efficiencies or save your organisation money, only to meet resistance and inertia from a significant portion of your team? Perhaps it is a new electronic prescribing module or a new communication platform to connect your healthcare teams.
Conversely, do you find yourself frustrated by your juniors unilaterally adopting new and unsanctioned digital technologies that have yet to be vetted by the appropriate authorities within your organisation?
It turns out the uptake of a new technology when introduced to a group of new users follows a very stereotypical and reproducible pattern that can be well described by the diffusion of innovations process (technology adoption lifecycle)1. Knowing where you and members of your team fit on the technology adoption curve will help you better manage team dynamics and effect real change within your organisation.
When introduced to a new group of users, the adoption of new technology typically follows a normal distribution (bell-shaped) curve with users falling into one of five groups (Fig 1):
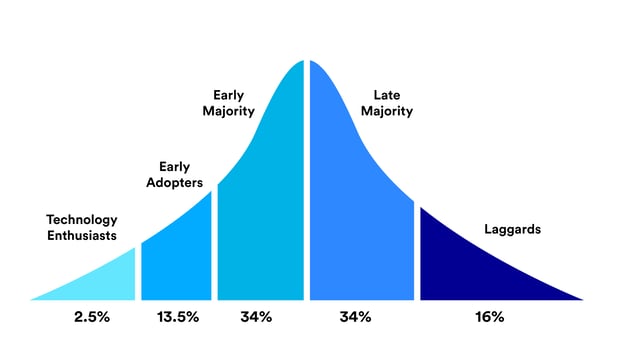
Fig 1. Technology Adoption Lifecycle
- Innovators/technology enthusiasts: These are the first to adopt a new technology. These individuals, constituting only 2.5% of the user base, like using technology for technology's sake rather than for the problem it solves. Think tech geeks.
- Early adopters/visionaries: The next group to jump on your new technology are the early adopters. These individuals adopt a new technology to give their organisation, their business or themselves a competitive edge. As such, they are happy to accept some shortcomings with the solution and are prepared to develop their own workarounds where necessary. Having the early adopters onboard is a good start to driving adoption by the rest of your team, but it is not enough.
- Early majority/pragmatists: Constituting 34% of users, these pragmatists tend to be more conservative. Typically, they are well established within your organisation, risk-averse, yet open to new ideas. Accordingly, these users typically seek references from their contemporaries (e.g. other pragmatists in different healthcare organisations) when adopting new technology, rather than seeking insights from the early adopters. In fact, pragmatists may view early adopters as impetuous and not informed of all the issues at hand within the organisation. Accordingly, the early majority are the key to onboarding the rest of your team and organisation. Your goal is to find a pragmatist with a significant pain point the software solution will solve.
- Late Majority: Again constituting 34% of the user base, the late majority are conservative, and generally dislike disruptive technology. Accordingly, they prefer to wait until the new technology has become a well and truly established standard before adopting.
- Laggards: Also known as sceptics, they constitute 16% of the market and often don’t want to use the solution at all costs, no matter what. After all, it’s the work of the devil right? Climate change ain’t real also. You get the picture. You can choose to ignore these individuals but at times they can undermine your efforts for change. A better strategy is to identify and be able to address their concerns and frame the discussion accordingly.
So how can you drive meaningful adoption of new health technologies?
Understanding where you and the rest of your team sit on the technology adoption curve is a good start. Finding your tech-savvy early adopters is a good next step, but to achieve meaningful adoption you really need the support of some key early majority users to get the rest of the team on board. These individuals will serve as the best referees for the rest of your organisation. Remember they see the benefit to change where appropriate but are risk-averse. Therefore, they will want to see you deliver the initiative as a total solution (i.e user onboarding, product education and training, policies and procedures, and appropriate support channels in place. Be respectful of both their needs and aversion to risk when initiating discussions.
The late majority and sceptics require cold hard evidence. Case studies and testimonials from other organisations that have successfully implemented the solution are a start. However, robust evidence supporting the software’s purported claims is ideal. When dealing with sceptics address their concerns head-on. Honesty is always the best approach. Also, be specific. Rather than saying ‘your team can be onboarded quickly’ say 'the team can be onboarded in ten minutes'.
2. Identify major obstacles to technology adoption rollout
Here are some of the major obstacles an organisation faces when implementing information technology rollouts:
- Lack of executive buy-in to the project.
- Failure to involve other key stakeholders in product rollouts such as frontline managers and clinical staff.
- Failing to allocate sufficient resources for change management: Successful technology adoption requires training, education and workflow redesign. Allow dedicated and protected time for staff to train in the new technology. Be mindful of staffing considerations - do you have shift workers, part-time staff or high administration staff turnover? If so, how will these users be onboarded?
- Are there technological barriers to implementation? Is a specific software integration required for user adoption?
- Review your workplace mobile device policies for M-health solutions: does your Bring-Your-Own-Device policy need updating for staff to be confident in using mobile solutions?
3. Adopt a change management mindset
Installing software on a healthcare workers computer or phone does not, in itself, change behaviour.The success of any technology implementation will, to a large degree, depend on your organisation’s effectiveness in change management: Here are some guiding principles to drive meaningful change:
- Identify key stakeholders: Understand the key people involved to make the rollout a success and involve them from the get-go. Get executive buy-in, but also ensure you have front line managers involved and supporting your initiative.
- Identify the technology champion within your organisation.
- Communicate your vision early to stakeholders and continue to provide feedback regularly.
- Help stakeholders identify the benefits for them in the work they do and focus on these outcomes during implementation.
- Allocate sufficient resources for in-depth training.
- Explain how the technology works within the context of their workflows and develop supporting policies.
- Develop support channels.
- Change takes time. Understand that clinician kickback is the norm. Medical staff are famously conservative. In fact, following an orderly and structured routine to patient care is an essential ingredient to minimising medical errors. Therefore in a doctor’s mind, changing workflows can introduce variation that could lead to patient harm. Understand and acknowledge workflow changes that will occur. Remember, change takes time.
There is evidence to support a strategic change management mindset to your implementation. According to Prosci’s Best Practices in Change Management projects with poor change management meet objectives less than 50% of the time. Projects with an excellent management approach achieve a 96% success rate.
4. Define success: Implementation does not mean adoption
Understand what success looks like. If long term adoption of your solution is the required outcome then ensure the right metrics are being assessed. Instead of asking ‘’was the project implemented on time and on budget?’’, focus on outcome metrics. Have the original problems we identified been solved with the implementation of the new software?
About Foxo
Foxo is a powerful clinical communication platform ready for rapid enterprise deployment. We’ve made onboarding simple at Foxo.
Curious about how we can improve healthcare outcomes for all stakeholders? Want more information about onboarding your team to Foxo or just want to reach out? We’d love to hear from you. Reach out to us at hello@foxo.com or register for a demo here.
References:
- Rogers, Everett (16 August 2003). Diffusion of Innovations, 5th Edition. Simon and Schuster. ISBN 978-0-7432-5823-4.
- Prosci’s Best Practices in Change Management 2018 edition